Studies Used By BYU Report - Scientific Evidence Of Efficacy Of Masks
Laura Sanger, Ph.D.
Twitter: @dunamis444hz
Note: Studies are numbered according to the reference page from the BYU report. The BYU report can be accessed at: https://brightspotcdn.byu.edu/7b/e7/75df64714f30a59c1ba7766a1c00/byu-covid-masks-abbott.pdf
Study #5) Howard, J. et al. (2020, April). Face Masks Against COVID-19: An Evidence Review. Preprints 2020, 1-8.
- This review selected by the BYU group is still under peer review.
- Howard et al. present a literature review on the “role of simple cloth masks and policies in reducing COVID-19 transmission.”
- They reviewed transmission characteristics of COVID-19 and state: “High viral titers of SARS-CoV-2 are reported in the saliva of COVID-19 patients. These titers have been highest at time of patient presentation and viral levels are just as high in asymptomatic or presymptomatic patients.” They reference Zou et al. (Study #73) which demonstrated similar viral load in an asymptomatic patient as patients who were symptomatic. The problem with relying on this study is that the findings were weakened because the sample size was one individual. The other study (Wӧlfel et. al. 2020) referenced by Howard et al. to support the above statement did not test asymptomatic patients. Wӧlfel et. al. 2020 found that the viral load in throat swabs was highest in all but one patient (N=9) at initial presentation BUT this was not true with viral load found in sputum (thick mucus from coughing). “Viral RNA concentration in sputum declined more slowly, with a peak during the first week of symptoms” in 4 out of 8 patients. Howard et al. (2020) fall prey to overstating the importance of Zou et al.’s findings of similar viral load in an asymptomatic patient. This should not be the only study used to draw this conclusion and has huge implications for public health interventions, such as mask mandates.
- They reviewed the filtering capability of masks and focused primarily on “source control” which they defined as “blocking droplets ejected by the wearer”. The primary argument for blocking droplets from healthy individuals is the belief that asymptomatic people transmit the virus similarly to infected people. But if this is not supported by the scientific data, then requiring everyone to wear a mask for source control is not necessary. Instead, masks worn by infected individuals would be indicated.
- Howard et al. reviewed the efficacy of masks based on RCT studies. One of the most frequently cited studies is MacIntyre et al. (2015) who evaluated the benefits and harms of mask usage. MacIntyre et al (2015) examined the rates of infection in 1607 Hospital Care Workers (HCW). It was the first research study to use a randomized control trial to test the efficacy of cloth masks vs surgical masks. The results suggested that penetration of cloth masks by virus particles was nearly 97% and by surgical masks 44%. The incidence of influenza-like illness and laboratory-confirmed virus was highest among those that wore cloth masks and these findings were statistically significant. This led the researchers to conclude “moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection.” Howard et al. pointed out that the control group in this study also wore masks and there was no control group consisting of HCW with no masks. This certainly would have strengthened the conclusions of whether cloth masks provided more protection than no masks, but it’s important to note that compliance with mask wearing among the control group was only 23.6%. While this study does not speak to community masking as ‘source control’ it does suggest that cloth masks are only 3% effective in filtering virus particles.
- Howard et al. reviewed studies on the impact of masks on community transmission. Two RCT studies conducted by Aiello et al. (2010, 2012) found that hand hygiene and mask usage combined reduced respiratory illnesses in shared living situations like dormitories and mitigated the spread of influenza A virus. However, Howard et al. did not mention an important finding within this study. Aiello et al. had three groups: mask and hand hygiene group, mask only group, and no mask group. Only the mask and hand hygiene group demonstrated a significant difference in reducing incidence rate of influenza A virus. The hand washing that took place in the mask only group and the no mask group was about the same and there was no significant difference found between the incidence rate in these two groups. The mask and hand hygiene group washed their hands significantly more than the other two groups. Aiello did not have a hand hygiene group only, but it would appear that the increase in hand hygiene is what played a substantial role in the differences found between groups.
-
BYU Report – There did not appear to be any bias or misrepresented concepts within the BYU report as it relates to the Howard review. The biases lie within the Howard review.
- “After infection, most people experience an incubation period where there are no symptoms – typically lasting 5 days, but sometimes lasting 15 days.” This is consistent with Howard et al. review.
- “It appears that the main way the virus is spread is through small droplets of moisture that are produced when a person exhales, talks, coughs, or sneezes.” This is consistent with Howard et al. review.
- “Researchers from hospitals, universities, the private sector, and government agencies have concluded that masks could be one of the most powerful and cost-effective tools to stop COVID-19 and accelerate the economic recovery.” This is consistent with Howard et al. review.
- “There is now convincing evidence from multiple controlled experiments…that wearing masks reduces the transmission of COVID-19 for healthcare workers and the public.” This is consistent with Howard et al. review.
- “Since then, multiple types of research have been conducted to evaluate how much masks can help, including laboratory tests, “natural experiments” where researchers compare effectiveness of different policies, and computer simulations based on what we know about transmission dynamics and the pathology of COVID-19.” This is consistent with Howard et al. review.
Study #6) Cheng, K. K., Lam, T. H. & Leung, C. C. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. The Lancet 0, (2020).
- This is not a scientific study but rather a brief paper written by public health officials contained in the Comment section of the Lancet Journal.
- BYU report uses this paper to state: “public masking works through ‘source control’”.
- Cheng et al. state “people often wear masks to protect themselves, but we suggest a stronger public health rationale is source control to protect others from respiratory droplets. This approach is important because of possible asymptomatic transmissions of SARS-CoV-2.” The study Cheng references to support this statement is Zou et al. (2020, Study #73 see below) which only has one asymptomatic participant in their study. One can hardly use this as supportive evidence for ‘source control’.
- The authors make the argument that mass masking is a “prevention paradox – i.e. interventions that bring moderate benefits to individuals but have large population benefits. Seatbelt wearing is one such example…masking can be compared to safe driving: other road users and pedestrians benefit from safe driving and if all drive carefully, the risk of road traffic crashes is reduced.” The problem with this argument is that there are virtually no negative side effects from wearing a seatbelt or driving safe, whereas masks can be a detriment to the social, psychological, and physical well-being of a person.
-
BYU report -
- “public masking works through ‘source control’” The primary problem with this article and the use of it in the BYU report is that it’s a circular argument that has no merit. BYU report makes their claim based on this article, but the article provides no direct scientific data. Instead this article points to another study, Zou et al. (2020), which only has one asymptomatic participant. So, in order to determine the legitimacy of the statement made in the BYU report, one has to dig through two other articles to prove the legitimacy. Was this obfuscation intentional? Are the BYU authors banking on the fact that most people won’t take the time to fact check their work? It’s too early to make that determination, but if this becomes a pattern in the BYU report, then I believe we can draw the conclusion that it was intentional.
Study #9) Abaluck, J. et al. (April 1, 2020) The Case for Universal Cloth Mask Adoption and Policies to Increase Supply of Medical Masks for Health Workers. https://papers.ssrn.com/abstract=3567438 (2020) doi:10.2139/ssrn.3567438.
- This was not a scientific study rather it was a white paper in which the authors discuss the “potential effectiveness of universal adoption of homemade cloth facemasks in mitigating” COVID-19.
- Authors make the statement “There is broad agreement about two crucial points: 1) people infected with the SARS-CoV2 virus can have minimal symptoms or can be completely asymptomatic. Thus, seemingly healthy people, including young people, are spreading the virus by transmitting it to others. 2) Masks, including cloth masks and surgical masks, have measurable efficacy at preventing infected people from transmitting viruses to others.” There is not broad agreement on these two points, in fact, my review of the scientific studies in this analysis demonstrates otherwise. The authors use a field briefing from the Japanese NIID regarding the Diamond Princess cruise to support their first point. However, upon reading the field briefing it states: “The proportion of asymptomatic cases observed aboard Diamond Princess [51%] is substantially higher than what has been reported elsewhere… Due to the lack of symptom presentation, it is not possible to infer when these cases were infected. Some may have been secondary cases within a given cabin. Some may have been infected before the quarantine began.” This statement does not support the claim by Abaluck that “healthy people are spreading the virus by transmitting it to others.” There is no way to determine from the findings of the field briefing that asymptomatic people were spreading the virus.
- “There is scientific evidence that homemade cloth masks can prevent viral transmission”, the authors reference Davies et al. 2013 (Study #89) and Rengasamy et al. 2010 (Study #44) to support their statement. The problem is that these studies actually do not recommend the use of cloth face masks in reducing the transmission of viruses. So, the authors twisted the findings from the studies they used to reference their statement.
- “Medical masks are extremely effective at preventing infected healthcare workers from transmitting the virus” (emphasis mine). This is not consistent with MacIntyre et al. (2015) findings in that medical masks allow 44% penetration of virus particles; extremely effective would more accurately describe N95 respirators. The use of adjectives in the above statement, reveals a pro-mask bias. [MacIntyre, C. R. et. al. (2015). A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open, 5(4).]
-
BYU report –
- “There is also recent evidence that masking is effective at state and national levels. In countries where public masking was common before the pandemic (where it was culturally normal for sick people to wear masks in public), COVID-19 had an initial daily growth rate of 10%, versus 18% in countries without such norms.” This statement is consistent with the article but does not include the text that directly follows this statement. Abaluck et al. state “This evidence is far from definitive: norms do not perfectly predict actual mask availability and use, these countries may have instituted other policies which contained the spread of the epidemic (such as widespread testing in South Korea), and infection rates are imperfectly measured and may appear higher in countries with more testing among other factors.” It’s interesting that the BYU report would stop short of including this important information highlighting the limitation of associating public masking with growth rates of COVID-19.
- “Infected individuals are most contagious during the day before first symptoms and in the few days after onset, meaning that people who feel completely healthy can spread the virus to loved ones and strangers.” While the white paper makes this claim, the supporting evidence used to make this claim DO NOT support it. Perhaps the BYU group did not read the articles Abaluck used to make this claim. Unfortunately, as I have quickly discovered, because the pandemic has become so politicized, it’s not prudent to just take papers/articles/experts at their word. It requires digging a few layers deep to actually read the studies to determine if the claims are accurate.
Study #11) Kenyon, C. (2020). Widespread use of face masks in public may slow the spread of SARS CoV-2: an ecological study. http://medrxiv.org/lookup/doi/10.1101/2020.03.31.20048652
- N = 49 countries met criteria in providing data across 3 variables of this study. 8 countries advocated wearing face masks in public (China, Czechia, Hong Kong, Japan, Singapore, South Korea, Thailand, and Malaysia).
- Methods - “assessed if there was ecological level evidence that countries that promoted face mask usage in public had a lower number of COVID-19 diagnoses per capita.” Variables considered in this study: 1) national policies promoting use of universal face masks in public regardless of symptoms (yes or no), 2) testing intensity (number of tests per million), and 3) age of epidemic (date first case diagnosed in each country).
- Results – face mask use was negatively associated with number of COVID-19 cases.
- Conclusions – “There are a number of countries in Western European such as Italy that have conducted intensive screening, contact tracing, isolation, social distancing and widespread lockdowns and yet have amongst the largest COVID-19 epidemics in the world. A striking omission from this response-list if we compare it to the responses in China and other Asian countries with lower COVID-19 incidence is that the widespread use of face masks in public was not promoted…Our analysis provides further evidence that this package should include widespread usage of face masks in public.”
- Limitations – the author stated “it is important to note that this association may be entirely explained by unmeasured confounders. A further limitation of our study was that we were unable to quantitate the intensity of face mask use per country. This resulted in a rather crude binary classification of face mask usage per country.” An ecological study is helpful to gain a high-level perspective of factors across countries contributing to differences in transmission rates, but it is inherently limited by the broad scope. As the author admitted, there are any number of factors they didn’t consider that could be contributing to the difference in transmission rate across countries. For example, in the Lombardi region of Northern Italy, a location particularly hit hard by the virus, there was a perfect storm so to speak, a high degree of pollution from industry, a large elderly population, a high incidence of smoking, and a new flu vaccine given to a vast majority of the population just prior to the pandemic. The flu vaccine contained dog tissue with coronavirus in it, making recipients more susceptible to COVID-19. (Dr. Dolores Cahill & Dr. Judy Mikovits). In Wuhan China, a quarantine was implemented within all of Wuhan to try to contain the virus. The Chinese people were not allowed to leave Wuhan. Hydroxychloroquine was used in Wuhan early in the outbreak and the doctors found it to be very effective. These are just a few examples of confounding variables that were not measured in this ecological study.
-
BYU report- used this study to make the following statements:
- “Up to one in three COVID-19 carriers show no symptoms at all (asymptomatic)” – there is a disconnect between the findings from Kenyon’s study and this statement. Perhaps it was a simple mistake by the BYU group to reference this study as it relates to their statement.
- “Likewise, the COVID-19 growth rate and mortality rate are lower in countries that required public masking.” This statement does not take into consideration the warning that the author provides that making an association between growth rates and mortality rates of COVID-19 with public masking does not account for unmeasured confounding variables.
Study #12) Anfinrud, P., Stadnytskyi, V., Bax, C. E. & Bax, A. (2020). Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. New England Journal of Medicine 382, 2061–2063.
- Researchers from the NIH performed a study in which they video recorded droplets generated by speech. They used a green laser light with a black box to capture the visual effect of the droplets released when a subject said “stay healthy” with no mask and with a mask.
- A “homemade cloth face mask” was used, but what is unusual is that the researchers used a “damp washcloth” as the mask. Why use a damp washcloth for this experiment, it does not generalize to the cloth masks worn by the public? It’s also inconsistent with the CDC recommendations for cloth mask use, which states, “people should not wear masks while engaged in activities that may cause the mask to become wet, like when swimming at the beach or pool. A wet mask may make it difficult to breathe.” (https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html) Why would the NIH conduct a study that is inconsistent with the guidelines of mask usage from the CDC? Do the water molecules of a damp mask make the washcloth denser, thus more effectively curbing the emission of saliva droplets?
- Limitations – researchers did not compare the release of droplets between a dry face mask and the damp face mask. Researchers “did not assess the relative roles of droplets generated during speech, droplet nuclei, and aerosols in the transmission of viruses” even though they state “the act of speaking generates oral fluid droplets that vary widely in size, and these droplets can harbor infectious virus particles.”
-
BYU Report –
- “Cloth masks can stop 90% or more of the dispersal of droplets carrying the virus.” This statement cannot be supported by this study.
- “These tiny droplets can travel many feet through the air and linger in the air or on surfaces for several minutes to hours after the infected person has left the area.” This was not addressed in this study.
- “There is clear evidence that face coverings reduce the spray of droplets produced during speaking, coughing and sneezing.” This study specifically measured droplets while speaking, not coughing or sneezing.
- “These are the reusable “home-made” masks that we have been recommended to wear when in public. Surprisingly, they have proven as or more effective as surgical masks and even N95 respirators in some circumstances to contain droplets and disperse air.” This study did not compare surgical masks and N95 respirators with the homemade mask. It has not been recommended to wear a damp washcloth as a "homemade mask".
- “The most recent studies have shown that even a basic covering is quite effective at limiting the spread of infectious respiratory droplets from speaking or coughing. The researchers tracked the number of droplets from the mouth of someone speaking with and without a mask, and their results showed that although cloth coverings certainly aren’t foolproof, they prevent most particles from traveling long distances where they could potentially infect others.” This is consistent with the study.
Study # 16) Roberge, R. J., Coca, A., Williams, W. J., Palmiero, A. J. & Powell, J. B. Surgical mask placement over N95 filtering facepiece respirators: Physiological effects on healthcare workers. Respirology 15, 516–521 (2010).
- N = 10 health Hospital Care Workers (HCW)
- Methods - Control study using same subjects carried out within 3 weeks of study phases. In the control study, there was no surgical mask (SM) placed over the N95 or N95EV. In study phase, surgical mask was placed over N95 and N95EV while subjects exercised at two different work rates (1.7 mph or 2.5 mph treadmill for 1 hour). HR, carbon dioxide, oxygen saturation, breathing rate, etc. were measured.
- Results – There was no significant difference when comparing N95/SM and the N95/EV/SM at both work rates on any of the measures. However, there was a significant difference in oxygen levels between control group and N95/SM at 1.7mph and N95/EV/SM at 2.5 mph. Additionally, “significantly lower exertion scores were reported for controls compared with N95/SM and N95/EV/SM” at both work rates, “suggesting a negative impact of the increased dead space provided by the SM.” The researchers acknowledged that both the oxygen levels and CO2 levels “were not harmonious” with OSHA workplace standards. But they dismiss the importance of this by saying that the OSHA standards are for an ambient workplace atmosphere. They note that while there were no statistically significant differences in the CO2 levels when SM was added to the N95’s, in two of the 10 subjects, increased levels of CO2 were found during the control trials and the study trials. This emphasizes “the great variability on the impact of N95 between individuals.” In other words, some people experience increased levels of CO2 when using an N95 respirator.
- Conclusion – “the use of SM as an outer barrier to increase the useful life of N95 FFR and N95 FFR/EV, did not result in a significantly increased physiological burden for HCW…Comfort scores, exertion scores and N95 moisture retention were not markedly impacted by this combination of respiratory protection.” This last statement is inaccurate and thus misleading. The results did, in fact, demonstrate there was a significant difference in exertion scores with the combination of respiratory protection as compared to controls.
- Limitations – The sample size was small (N=10). This study did not compare the change in HR, carbon dioxide, oxygen saturation, breathing rate etc. with an N95 vs no mask. The researchers were misleading in their conclusion section which leads other researchers, who cite their conclusions, to unknowingly make the same mistake.
-
BYU report –
- “Masks are highly safe, with only minor and uncommon side effects.” This article does not support this statement. Researchers found that CO2 levels were increased in 20% of the participants and oxygen levels were significantly reduced when a surgical mask was layered upon an N95.
- “Several mild and rare side effects have been identified, including skin irritation, headaches and general discomfort in a minority of users.” This article did not address these side effects.
- “Despite widespread concern on social media and in the news, there is no evidence that masking causes dangerous hypoxia (low oxygen) or hypercapnia (high carbon dioxide) in healthy individuals, even when multiple masks are layered on top of each other.” Oxygen levels were reduced but the respirators were only worn for one hour, it’s possible hypoxia could have set in with an extended duration. Carbon dioxide was increased in 2 of 10 participants with the use of N95.
- “The current literature and industry practices indicate that there is very minimal risk of hypoxia and hypercapnia when wearing N95 respirators, and even when a surgical mask is layered on top there appears to be no physiological burden or significant change in oxygen or carbon dioxide levels.” This is not accurate based on the findings, but here is an example of how the misleading statements in the conclusion section of this study, led the BYU researchers to make the same mistake.
Study #33) MacIntyre, C. R. et al. (2016). Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open 6, e012330.
- N = 245 index cases with influenza-like illness (ILI)
- Methods - A randomized controlled trial (RCT) was conducted with 245 index cases and their household contacts. 123 index cases and their household contacts were in the intervention (mask) group, and 122 index cases and their household contacts were in the control (no-mask) group. For those index cases in the intervention group, they were asked to wear a mask when they were in the same room as household contacts. Mask use by other household contacts was not required and not reported. Illness outcomes were measured of household contacts for clinical respiratory illness (CRI), ILI, and laboratory confirmed viral respiratory infection. If household members began to develop symptoms, they were to report this to the researchers.
- Results – there was no statistical significance between the mask group and the no-mask group. “There was no association between mask use by the index cases and rates of infectious outcomes in household members. Although the risks of CRI, ILI, and laboratory confirmed viral infections were lower in the mask arm, the difference was not statistically significant.” It’s important to note that the researchers ran additional analyses to compare those in the intervention group that actually wore a mask (65%) with the control group and there was a significant lower rate of CRI in the mask group.
- Conclusions – “Masks are commonly recommended as source control for patients with respiratory infections to prevent the spread of infections to others, but data on the clinical efficacy of this approach are sparse. We did not find a significant benefit of medical masks as source control, but rates of CRI and ILI in household members were consistently lower in the mask [group] compared with the control [group].”
- Limitations – there are few limitations with this study. It was a robust, clearly defined study using randomized selection between the intervention group and the control group. This is a high-quality research study.
-
BYU report - used this study in conjunction with others, but often in a way that is not consistent with the content of the study. For example, the report states:
- “cloth masks primarily provide source control rather than external protection, though some level of external protection appears likely depending on the fabric and the way the mask is worn.” This study did not use cloth masks.
- “Because only fitted respirators (the finest meshed masks) provide reliable protection from external droplets and viral particles.” This study did not address fitted respirators.
- “Because masks have been used by medical professionals for centuries, there is a large body of scientific evidence about their performance and safety.” This is not consistent with MacIntyre et al. (2016) state “Cloth and medical masks were originally developed as source control to prevent contamination of sterile sites by the wearer in operating theatres (OTs); however, their effectiveness in preventing surgical site infections is yet to be proven. In other clinical trials, masks were either used by both sick patients (index cases as source control) and their household members or only by household members. Most of these studies failed to show any efficacy of mask use in preventing spread of infections from the sick individuals.” The BYU report suggests that this study provides evidence for the performance and safety of masks. It does not address safety at all, and speaks more about the inconclusive findings regarding the performance of masks.
- “in past situations with less virulent diseases and lower levels of community spread, experts expressed caution when extending the successes of mask-wearing to large interpersonal contexts such as schools or healthcare settings.” This is consistent with the findings of the study.
Study # 41) Leung, N. H. L. et al. (2020, May) Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine 26, 676–680.
- N = 246 participants. Participants were recruited year-round from March 2013 to May 2016. 122 participants were randomized to wear a mask during exhaled breath collection, 124 randomized to not wear a mask. Of these 246 participants, 123 had at least one respiratory virus (n = 17 seasonal coronavirus (not COVID-19), n = 43 influenza, n = 54 rhinovirus).
- Methods - Researchers examined the importance of aerosol routes and respiratory droplets in the transmission of coronavirus, influenza, and rhinovirus. They “tested viral shedding in nasal swabs, throat swabs, respiratory droplet samples and aerosol samples and compared the latter two between samples collected with or without a face mask.” Participants provided exhaled breath samples for 30 minutes.
- Results – Viral RNA was identified from respiratory droplets and aerosols for all 3 viruses when participants were not wearing a mask during the breath samples. Coronavirus was detected in droplets in 30% of participants, and in aerosols in 40% of participants, but did not detect any virus in respiratory droplets or aerosols from participants with a face mask. Their findings were statistically significant for aerosols and showed a trend toward reduced detection for droplets.
- A subset of participants did not cough during their exhaled breath collection (n= 37 without a mask, n = 42 with a mask). “In a subset for coronavirus (n=4), we did not detect any virus in respiratory droplets of aerosols from any participants.” This would suggest that coronavirus is not as easily detected when coughing is not present.
- Conclusions – researchers demonstrated the efficacy of surgical masks to reduce coronavirus detection and viral copies in large respiratory droplets and in aerosols. “This has important implications for control of COVID-19, suggesting that surgical face masks could be used by ill people to reduce onward transmission.” But it’s important to note “among the samples collected without a face mask, we found that the majority of participants with influenza virus and coronavirus infection did not shed detectable virus in respiratory droplets or aerosols.” (emphasis mine)
- Limitations – researchers stated “the major limitations of our study was the large proportion of participants with undetectable viral shedding in exhaled breath for each of the viruses studied.” Also, the researchers were studying seasonal coronavirus and not COVID-19.
-
BYU report –
- “For example, one of the most definitive studies on viruses and face masks found a 90% reduction in influenza viruses after breathing through a mask and a complete removal of coronaviruses.” This is not an accurate statement and stops short of the full picture, let me explain. The researchers found virus detection from droplets in 26% of influenza participants which reduced to 4% when masks were used. This is an 85% reduction (4/26 = 0.15, 1-0.15 = 0.85 or 85%) and was statistically significant. The researchers found virus detection from aerosols in 35% of influenza participants when no masks were used and 22% when masks were used. This is a 37% reduction which was not statistically significant. It is true that when surgical masks were used, no virus detection was found from droplets or aerosols with coronavirus participants, but only the finding with aerosols was statistically significant. From the coronavirus participants who did not cough during the exhaled breath collection, no virus detection was found, suggesting that minimal symptoms or no symptoms reduces coronavirus detection. The BYU report failed to take into consideration the whole picture. Instead, when we consider all the results together, we can see why the researchers concluded that surgical masks may be used to reduce the transmission of COVID-19 when worn by ill people.
Study #44) Rengasamy, S., Eimer, B. & Shaffer, R. E. (2010). Simple Respiratory Protection—Evaluation of the Filtration Performance of Cloth Masks and Common Fabric Materials Against 20–1000 nm Size Particles. Annals of Occupuational Hygiene 54, 789–798.
- Research was conducted on the effectiveness of woven cloth masks for the transmission of influenza virus.
- Methods – Household fabrics and cloth masks were challenged with a polydisperse as well as monodisperse particles in the 0.02 - 1μm range in diameter. This is similar to the size of most virus particles. Fabrics used: sweatshirts, T-shirts, towels, scarves, and cloth masks were used for the aerosol penetration tests. N95 respirator was used for comparison with the household fabrics.
- Results – “Average penetration levels for the three different cloth masks were between 74 and 90%, while N95 filter media controls showed 0.12%...the three sweatshirts showed 40% penetration level…the other two models showed penetration levels in the 70-82% range…T-shirts showed penetration levels >86%...average penetration levels for the three different model towels and scarves were in the 60-66% and 73-89% ranges, respectively.”
- Conclusions – “The use of fabric materials may provide only minimal levels of respiratory protection to a wearer against virus-size submicron aerosol particles (e.g. droplet nuclei). This is partly because fabric materials show only marginal filtration performance against virus size particles when sealed around the edges. Face seal leakage will further decrease respiratory protection offered by fabric materials…Thus the use of improvised fabric materials may be of some value compared to no protection at all when respirators are not available.”
-
BYU report –
- “This is why masks have long been recommended for individuals with respiratory infections”. The findings of this study do not support the BYU statement, rather the findings would only support it if the “mask” were an N95 respirator.
Study #89) Davies, A. et al. (2013) Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic? Disaster Medicine and Public Health Preparedness, 7, 413–418.
- N = 21 healthy adults
- Methods – This study assessed whether improvised masks could provide protection for wearers from infected individuals. Common household materials were used to make masks and were tested for filtration efficiencies from high concentrations of bacterial and viral aerosols (Bacillus atrophaeus 0.95 – 1.25μm, Bacteriophage MS2 0.023μm). Additionally, pressure drop across each of the materials was measured to determine the comfort and fit of the masks. “To determine the effect of homemade and surgical masks in preventing the dispersal of droplets and aerosol particles produced by the wearer, the total bacterial count was measured when the volunteers coughed wearing their homemade mask, a surgical mask, and no mask.”
- Results – The surgical mask was generally more effective in reducing the number of micro-organisms expelled than the homemade masks, especially with the smaller particles. Statistical tests comparing the proportion of particles greater than 4.7μm and less than 4.7μm found that the homemade mask did not significantly reduce the number of particles emitted. But the surgical mask did have a significant effect.
- Conclusion – “An improvised face mask should be viewed as the last possible alternative if a supply of commercial face masks is not available…but it would be better than no protection…these masks would provide the wearer little protection from microorganisms from other persons who are infected with respiratory diseases. As a result, we would not recommend the use of homemade face masks as a method of reducing transmission of infection from aerosols.”
-
BYU Report –
- “though some level of external protection appears likely depending on the fabric and the way the mask is worn”. This is consistent with the findings.
- “In the current pandemic, the consensus is growing that public masking should be used in combination with other efforts rather than not at all.” This is also consistent with the findings; the cloth masks did provide some level of protection but it’s interesting that the BYU report did not mention the main findings from the study which I have highlighted above. Again, this might be evidence of a pro-mask bias among the BYU team.
Study #92) MacIntyre, C. R. et al. (2009) Face Mask Use and Control of Respiratory Virus Transmission in Households. Emerging Infectious Diseases 15, (2), 233-241.
- N = 290 adults from 145 families; 47 households in surgical mask group, 46 households in P2 (similar to N95) mask group, and 52 households in the control group (no-mask)
- Methods – participants were randomly assigned to each group. Adults were chosen if they were healthy but have a sick child with a fever and respiratory symptoms. Adults were instructed to wear the masks anytime they were in the same room as the sick child. Participants were also instructed how to wear and dispose of the masks. Researchers contacted participants by the phone daily to assess adherence to mask use and if symptoms had developed. Influenza like illness (ILI) was defined by the “presence of fever, feeling feverish or a history of fever, ≥ 2 symptoms (sore throat, cough, sneezing, runny nose, nasal congestion, headache), or 1 of the symptoms listed plus laboratory confirmation of respiratory viral infection.” It’s important to note that in this study, masks were worn by the healthy adult.
- Results – ILI was reported in 22.3% (21/94) of the adults in the surgical mask group, 15.2% (14/92) in the P2 group, and 16% (16/100) in the control group. These findings demonstrate that the highest incidence rate of transmission was among the surgical mask group, not the no-mask control group. “Even intention-to-treat analysis using ILI outcome shows no significant difference between the groups.”
- Conclusions – “The key findings are that ≤ 50% of participants were adherent with mask use and that the intention-to-treat analysis showed no difference between arms. Although our study suggests that community use of face masks is unlikely to be an effective control policy for seasonal respiratory diseases, adherent mask users had a significant reduction in the risk for clinical infection. Another recent study that examined the use of surgical masks and handwashing for the prevention of influenza transmission also found no significant difference between the interventions [groups]…Therefore, although we found that distributing masks during seasonal winter influenza outbreaks is an ineffective control measure characterized by low adherence, results indicate the potential efficacy of masks in contexts where a larger adherence may be expected, such as during a severe influenza pandemic or other emerging infection…We urge caution in extrapolating our results to school, workplace or community contexts, or where multiple, repeated exposures may occur…”
- Limitations – MacIntyre et al. generally design robust randomized clinical trials with no exception here, therefore, I find their work to be the most scientifically sound of the studies included by the BYU report. However, a limitation in this study surfaces in the data provided in Table 4. First, they make a minor error in reporting the incidence of ILI in the surgical group as per the data they reported in the body of their paper. But more importantly, if you notice the highlighted values; the total number of laboratory-confirmed infections in the control group is only 3% (3/100), whereas in the surgical mask group it’s 6% (6/94), and 9% in the P2 mask group (8/92). These findings taken together with the incidence of ILI demonstrate that healthy adults are better off not wearing a mask when caring for a sick child. But the researchers failed to draw this important conclusion regarding the efficacy of masks used in household settings. The only mask that performed better than no mask at all with regard to ILI was the P2 mask, but realistically, how many people are going to wear a P2 (similar to N95) mask around their house. The researchers concluded that there is potential efficacy for masks worn by healthy adults in a pandemic because there may be greater adherence to wearing a mask. I disagree with their reasoning, in a pandemic, community wide mask mandates using N95 or P2 masks is simply not feasible. Furthermore, their own data demonstrate that a healthy adult is less likely to become infected with a respiratory illness if they use no mask at all.
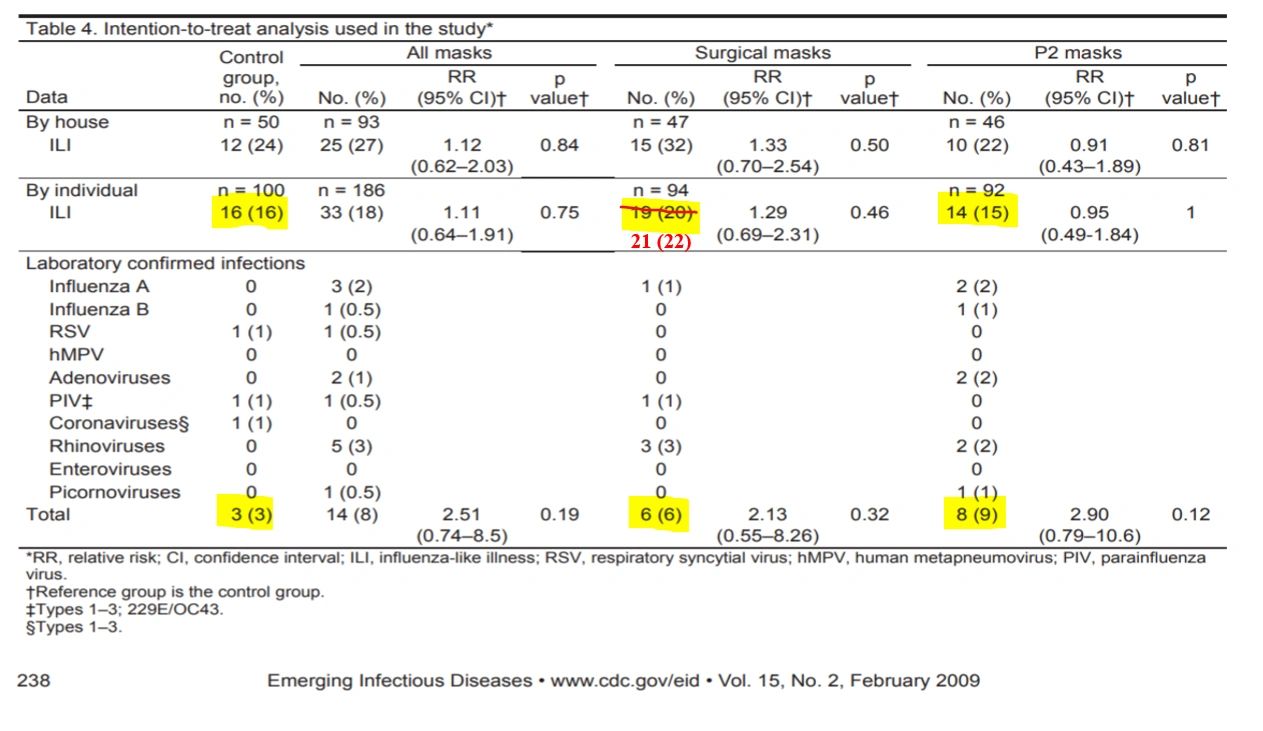
Table 4 adjusted by Laura Sanger, Ph.D. to correct for error by MacIntyre et al. (2009).
-
BYU report –
- “They emphasized that other preventative measures such as physical distancing, washing hands, and staying home would be more effective than purely relying on masks.” This is consistent with the study.
- “In the current pandemic, the consensus is growing that public masking should be used in combination with other efforts rather than not at all.” Once again, from the data reported in this research study, no mask at all would be better at reducing the rate of laboratory confirmed infection. In the current pandemic, we are being told to use cloth masks (often homemade) which the efficacy of such masks IS NOT supported by this study. The only mask that could prove helpful based on the findings of this study is a P2 or N95 mask.
Study not included in BYU report - MacIntyre, C. R. et. al. (2015). A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open, 5(4), 1-10.
- This is a seminal study on the efficacy of cloth masks; it was the first RCT. “The aim of this study was to determine the efficacy of cloth masks compared with medical masks in HCW’s working in high-risk hospital wards, against prevention of respiratory infections.”
- N = 1067 HCW
- Methods – Hospital wards were randomized to medical masks, cloth masks, or control group (standard practice which included some mask wearing). Participants were followed for 4 weeks in their mask usage and an additional week for symptom assessment. Participants were assessed for Clinical respiratory illness (CRI; 2 or more respiratory symptoms or 1 respiratory symptom and 1 systemic symptom), ILI (fever ≥38°C plus 1 respiratory symptom), and laboratory-confirmed respiratory virus infection.
- Results – Findings show that “the rates of CRI was highest in the cloth mask arm, followed by the control arm, and lowest in the medical mask arm. The same trend was seen for ILI and laboratory tests confirmed viral infections…In intention-to-treat analysis, ILI was significantly higher among HCWs in the cloth masks group compared with the medical masks group.”
- Conclusions – “The physical properties of a cloth mask, reuse, the frequency and effectiveness of cleaning, and increased moisture retention, may potentially increase the infection risk for HCWs. The virus may survive on the surface of the face masks. When we analysed all mask-wearers including controls, the higher risk of cloth masks was seen for laboratory-confirmed respiratory viral infection.”
- BYU Report - While this study was included in the studies the BYU group reviewed, they did not include it in their July 19th report. I find this interesting, especially given the study does not support the efficacy of cloth masks. Is this why it was excluded from the BYU report?